Denial Management
Turning The Challenge of Denials into Opportunities
Denial management plays a crucial role within healthcare organizations, ensuring a healthy revenue cycle while maximizing collections. Healthcare Chaos Management leverages decades of payer experience, advanced algorithm modeling, and cutting-edge AI technology to transform denials into opportunities for improvement and growth, ensuring that healthcare providers receive appropriate reimbursement for their services.
What is a Denial?
A denial occurs when an insurance payer refuses to pay a claim in full or in part. Denials can be costly and time-consuming, leading to delayed or lost revenue for healthcare providers.
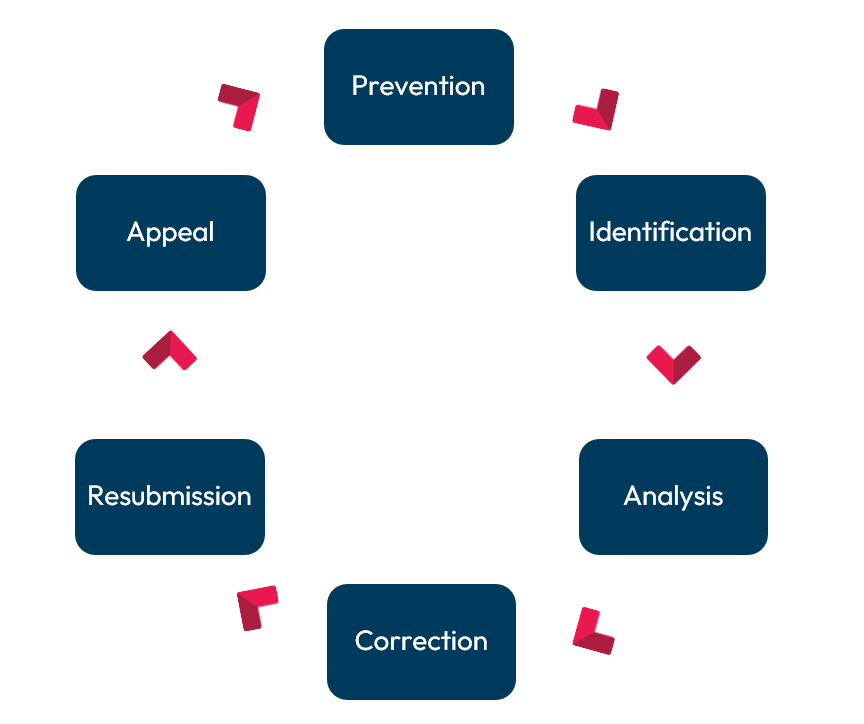
Denial Management Process
Why is Denial Management Important?
Effective denial management is essential for several reasons:
- Revenue Optimization: By effectively managing denials, healthcare organizations can identify and rectify issues that lead to claim rejections, ensuring that all eligible services are reimbursed appropriately.
- Cash Flow Improvement: Timely and efficient denial management processes can help expedite the resolution of denied claims, ensuring a steady cash flow and reducing financial strain.
- Cost Reduction: By proactively addressing denial trends and implementing strategies to prevent future denials, providers can reduce the administrative burden and associated costs of claims management.
- Enhanced Productivity: Denial management processes that are streamlined and efficient enable staff to focus their time and resources on more productive activities, such as patient care and revenue-generating tasks, rather than on resolving billing and claims issues.
- Improved Patient Satisfaction: Efficient denial management leads to faster resolution of billing issues, resulting in more accurate and timely patient statements. This, in turn, enhances patient satisfaction by reducing billing errors and providing clear communication about financial responsibilities.
Denial Management Strategies
Successful denial management requires a multi-faceted, technology-driven approach:
- Process Optimization: Streamline claims submission processes to reduce administrative delays and ensure timely filing. Implement standardized procedures and workflows to improve efficiency and accuracy in claim processing.
- Technology Utilization: We leverage advanced denial management software, AI, and analytics tools to streamline processes, identify trends, and prioritize denials. These technologies automate the identification of patterns and provide actionable insights to address the root causes of denials.
- Staff Training: While automation handles many tasks, we ensure that the HCM employees are well-trained in coding, billing, and insurance regulations. This training minimizes errors and enhances the effectiveness of our AI tools by ensuring high-quality input data.
- Continuous Improvement: We use AI and machine learning to continuously monitor and evaluate denial rates. These tools adapt and improve over time, implementing changes to enhance performance and prevent future denials. Implement feedback mechanisms and key performance metrics to measure effectiveness and drive continuous improvement efforts.
Expertise and Advanced Modeling
Our team combines deep expertise with sophisticated algorithm modeling to ensure quicker resolutions and higher success rates in appeals. This focused approach has led to:
- Reduced Days in Accounts Receivable (A/R): Efficient processes ensure faster resolution of denied claims, improving cash flow and reducing financial strain.
- Identification of Upstream Opportunities: By analyzing denial patterns, we pinpoint root causes and implement proactive measures to prevent future denials.
- Reduction in Cost-to-Collect: Streamlined workflows and automated processes decrease the costs associated with managing and appealing denials.
- Increased Revenue: Our targeted strategies and efficient claim management processes maximize reimbursement rates, leading to significant revenue growth for healthcare organizations.
Comprehensive Workflow Integration
Our denial management process is seamlessly integrated into your existing revenue cycle operations, ensuring minimal disruption and maximum efficiency.
- Improved clean claim rates
- Reduced time to payment
- Fewer claims rejections
Continuous Improvement
We believe in continuous improvement and regularly review the outcomes of our denial management efforts to refine and enhance our processes.
- Ongoing Performance Monitoring: By tracking denial reasons and outcomes, we identify areas for improvement and adapt our strategies accordingly.
- Feedback Loop: Insights gained from analyzing denial patterns are fed back into our systems, ensuring that our approach evolves with the changing healthcare landscape.
Learn More
Discover how Healthcare Chaos Management can transform your denial management process and optimize your revenue cycle.